Meniscus
Injury
The knee is one of the most complex joints in the human body. As many sports place extreme stress on the knee, it is also one of the most common sites for sports injuries.
Anatomy
As the knee is a hinge joint, it is structured to perform two principal actions, flexion (bending) and extension (straightening). The muscles which act at the knee are predominantly the quadriceps (extension) and the hamstrings (flexion).
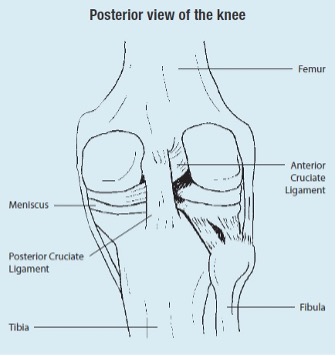
Meniscus tear is a common injury that affects the knee joint. The meniscus are ‘C’ shaped discs, made of tough cartilage called fibrocartilage.
They are positioned on the tibial plateau (top surface of the shin bone) between the tibia (shin bone) and the femur (thigh bone) and are important for distributing load and absorbing shock at the knee joint. There are two menisci within each knee joint.
Risk
Meniscal tears can occur in isolation or in combination with a ligamentous injury. The meniscus in the knee is usually damaged by a twist occurring on a slightly flexed knee. A partial or total tear of a meniscus may occur when a person quickly twists or rotates the upper leg while the foot stays planted. Repeated or prolonged squatting can also tear the meniscus.
Meniscal tears can be degenerative or traumatic. Degenerative tears occur as part of progressive wear in the whole joint or as a result of habitual, prolonged squatting. In the older adult, the tear may be due to a natural degeneration of the menisci that occurs with age. The traumatic type of injury is quite common in the athletic setting. The medial meniscus is more commonly affected than the lateral meniscus, whilst tears in both menisci are much less common.
Prevention
- Undertaking training prior to competition to ensure readiness to play.
- Warming up, stretching and cooling down.
- Undertaking fitness programs to develop strength, balance, coordination and flexibility.
- Gradually increasing the intensity and duration of training.
- Allowing adequate recovery time between workouts or training sessions.
- Wearing the right protective equipment including footwear. A good pair of shoes will help to keep knees stable, providing adequate cushioning, and supporting knees and the lower leg during the running or walking motion.
- Checking the sporting environment for hazards.
- Drinking water before, during and after play.
- Avoiding activities that cause pain.
Signs and Symptoms
Pain is usually experienced when a meniscus is injured, particularly when trying to straighten, bend or twist the knee. If the tear is tiny, the meniscus stays connected to the front and back of the knee. If the tear is large however, the meniscus may be left only slightly intact. Severe, intermittent sharp pain may occur, and is localised to that side of the joint. This results from part of the tear catching between the articular surfaces of the tibia and femur, blocking full extension of the knee, causing a ‘locking’ sensation.
Swelling may occur soon after the injury or several hours later as a result of inflammation. Complaints of clicking, popping or locking of the knee may also follow a meniscus injury. In some cases, after the initial swelling and pain, the joint settles down and normal activities can be resumed. This may be because the tear in the meniscus is small or the flap does not affect joint mechanics.
Immediate Management
The immediate treatment of any soft tissue injury consists of the RICER protocol – rest, ice, compression, elevation and referral. RICE protocol should be followed for 48–72 hours. The aim is to reduce the bleeding and damage within the joint. The knee should be rested in an elevated position with an ice pack applied for 20 minutes every two hours (never apply ice directly to the skin). A correctly sized compression bandage should be applied to limit swelling and bleeding in the joint.
The No HARM protocol should also be applied – no heat, no alcohol, no running or activity, and no massage. This will ensure decreased swelling and bleeding in the injured area.
A sports medicine professional should be seen as soon as possible to determine the extent of the injury and to provide advice on treatment required. A sports medicine professional may perform a physical examination and take x-rays of the knee. An MRI test may be recommended to confirm the diagnosis. An arthroscopy may also be used to help diagnose and treat a meniscal tear.
Rehabilitation and Return to Play
If the tear is minor and the pain and other symptoms cease, a muscle-strengthening program may be recommended. A large tear produces a flap of meniscus that may interfere with normal joint mechanics. The torn flap of meniscus can cause further damage leading to greater risk of degenerative arthritis. Due to the nature of the tear that the menisci can suffer, repair of the meniscus can be a complicated issue.
A meniscal tear that is symptomatic (painful with activities of daily living) may need to be addressed surgically. If so, this is now done by arthroscopic (keyhole) surgery which allows the surgeon to remove the flap and smooth off the surface of the meniscus, or if possible repair the torn meniscus. This will leave ‘normal’ structures and decrease the likelihood of degenerative arthritic changes.
The major goal of the rehabilitation program is to normalise walking, normalise pain-free range of motion, prevent muscle wastage and maintain cardiovascular fitness. Rehabilitation after meniscus surgery should focus on early mobilisation of the knee joint and quadriceps and hamstring strength. Weight bearing exercises should be added as directed by a sports medicine professional. Regardless of the form of surgery, rehabilitation usually includes walking, bending the legs, and doing exercises that stretch and build the leg muscles.
Return to play after a meniscal injury is expected. The timing is variable and depends on the injury, treatment and rehabilitation protocol. In many cases, return to sport can be as soon as two to three weeks or as long as six to eight weeks. Strapping, or taping, can provide an added level of support and stability to weak or injured knees during the rehabilitation process.
Acknowledgements
Sports Medicine Australia wishes to thank the sports medicine practitioners and SMA state branches who provided expert feedback in the development of this fact sheet.
Images are courtesy of www.istockphoto.com
Always Consult a Trained Professional
The information above is general in nature and is only intended to provide a summary of the subject matter covered. It is not a substitute for medical advice and you should always consult a trained professional practising in the area of sports medicine in relation to any injury. You use or rely on the information above at your own risk and no party involved in the production of this resource accepts any responsibility for the information contained within it or your use of that information.
