Gastrocnemius
(Calf) Strain
The Gastrocnemius muscle is a powerful superficial muscle located at the back of the lower leg and is involved in standing, walking, running and jumping.
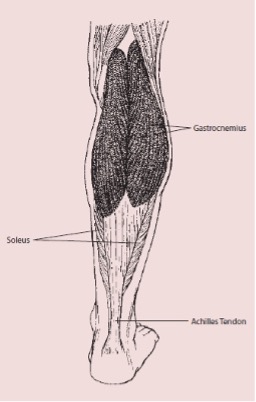
Often referred to as the calf muscle, it is located behind the tibia (shin bone) and works across both the knee and ankle joints. It extends from the base of the femur (thigh bone) behind the knee, to the calcaneus (heel bone). The muscle inserts into the Achilles Tendon along with other muscles. The muscle’s main roles are to plantar flex the foot (point toes away from yourself ) and to assist in flexing (bending) the knee.
Risk
The Gastrocnemius is commonly injured in sports which require quick acceleration from a stationary position and quick halts in movement, i.e., tennis or squash. In many such cases the injury is caused through sudden eccentric overstretch, i.e., the muscle is contracted yet lengthened forcibly and abruptly. An example of this is when an athlete runs onto a kerb and the ankle drops suddenly into dorsiflexion (point toes upward toward yourself ).
The most common place to incur this injury is at the muscular tendinous junction or MTJ of the Gastrocnemius – roughly halfway between the knee and the heel.
A calf strain may also be more likely in athletes who have tight calf muscles.
Prevention
- Keeping calf muscles strong so they can absorb the energy of sudden physical stress.
- Stretching out calf muscles before physical activity, i.e., calf raises. Gradually including weights or additional resistance over time.
- Learning the proper technique for exercise and sporting activities. This will decrease stress on all muscles, including calf muscles.
- Undertaking training prior to competition to ensure readiness to play.
- Undertaking fitness programs to develop strength, balance, coordination and flexibility.
- Gradually increasing the intensity and duration of training.
- Allowing adequate recovery time between workouts or training sessions.
- Wearing the right protective equipment including footwear.
- Checking the sporting environment for hazards.
- Drinking water before, during and after play.
- Avoiding activities that cause pain. If pain does occur, discontinuing the activity immediately and commencing RICER.
Signs and Symptoms
- A sudden pain at the back of the leg, particularly at the muscular tendinous junction.
- Difficulty in contracting the muscle or standing on tiptoe.
- Pain and swelling or bruising in the calf muscle.
- Pain on resisted plantar flexion or contracting the muscles against resistance.
- If the soleus muscle is damaged, pain might be incurred lower in the leg and, when contracting the muscle against resistance, with the knee bent.
Gastrocnemius strains are graded in three categories according to their severity.
|
Grade |
Description |
|
1 (mild) |
Sharp pain (during or after activity), may be unable to continue activity. Return to play – 10 to 12 days |
|
2 (moderate) |
Unable to continue activity. Return to play – 16 to 21 days |
|
3 (severe) |
Severe pain at junction between Achilles tendon and belly of the muscle. Return to play – approx. 6 months, if surgery is required. |
Immediate Management
The immediate treatment of any soft tissue injury consists of the RICER protocol – rest, ice, compression, elevation and referral to a sports medicine professional. RICE protocol should be followed for 48–72 hours. The aim is to reduce the bleeding and damage in the muscle. The leg should be rested in an elevated position with an ice pack applied for 20 minutes every two hours (never apply ice directly to the skin). A correctly sized compression bandage should be applied to limit bleeding and swelling in the injured area.
The No HARM protocol should also be applied – no heat, no alcohol, no running or activity, and no massage. This will ensure decreased bleeding and swelling in the injured area.
Rehabilitation and Return to Play
As pain decreases, gentle exercise and stretching can usually begin in addition to treatment recommended by a sports medicine professional. Rehabilitation should be conducted with caution and under the supervision of a sport medicine professional due to the risk of injury recurrence. Recovery can often be quite a slow process.
Acknowledgements
Sports Medicine Australia wishes to thank the sports medicine practitioners and SMA state branches who provided expert feedback in the development of this fact sheet.
Images are courtesy of www.istockphoto.com
Always Consult a Trained Professional
The information above is general in nature and is only intended to provide a summary of the subject matter covered. It is not a substitute for medical advice and you should always consult a trained professional practising in the area of sports medicine in relation to any injury. You use or rely on the information above at your own risk and no party involved in the production of this resource accepts any responsibility for the information contained within it or your use of that information.
