Eye
Injuries
Sports injuries to the eye can be minor, such as external bruising, to catastrophic, such as loss of vision. With vigilance, and proper preventive measures, the number of sports related eye injuries can be dramatically reduced.
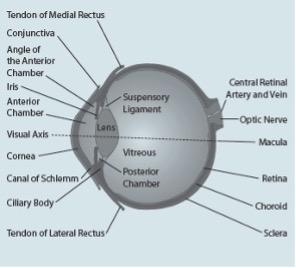
The eyeball and its lens focus light from an image onto the retina. The amount of light entering the eye is controlled by the pupil, which opens and closes. The light sensitive cells on the retina detect the electrical impulses and they travel to the brain. Anatomy of the eye includes lacrimal gland, cornea, conjunctiva, uvea (iris, choroid and ciliary body), lens, blood supply, retina, vitreous and optic-nerve.
Risk
While the incidence of sports related eye injuries is low, their severity is usually quite high as injuries to the eye can result in permanent eye damage and loss of eyesight. Research has shown that 30% of sports related eye injuries in children have the potential for permanent loss of eyesight.
A blow to the eye from sporting equipment, fingers or balls can lead to injuries ranging from lid haemorrhages or lacerations, corneal abrasions, retinal detachments and hyphaema (bleeding inside the eye) to permanent loss of eyesight.
Research indicates that beginners are more prone to eye injuries than intermediate or advanced players as beginners are yet to learn or refine the skills necessary to master the specific sport and play safely.
Sports can be classified on the basis of high risk, moderate risk and low risk for eye injury.
Note: the sports listed below are in alphabetical order and in no way indicate a greater or lesser incidence or risk of eye injury.
High risk sports
Involve small, high speed, dense projectiles in close proximity to athletes. Examples include:
Sports with small, high velocity projectiles:
- Air rifle
- Paintball
Sports with hard, dense projectiles, fingers at close contact, or the use of a bat or stick:
- Badminton
- Baseball/softball
- Basketball
- Cricket/indoor cricket
- Fencing
- Field hockey
- Ice hockey
- Lacrosse
- Squash/racquetball
- Tennis
Moderate risk sports
Involve a high speed ball or puck, the use of a bat or stick, close aggressive physical body contact with intentional or unintentional collisions or a combination of these factors.
Examples include:
- American football (Gridiron)
- Archery/darts
- Australian Rules football/rugby union/rugby league
- Soccer/volleyball
- Water polo
Low risk sports
Do not involve a thrown or hit ball, a bat or stick, or close aggressive play with physical body contact.
Examples include:
- Athletics
- Cycling
- Rowing/canoeing
- Skiing
- Swimming/diving
- Water skiing
Prevention
Most eye injuries in sport are preventable. Minimising the severity and incidence of eye injuries in sporting environments is based on the following three principles.
- Modifying rules in junior sport to limit the risk and ensure safe play.
- Developing coaching procedures and practices that encourage safe play.
- Where appropriate, wearing protective eyewear, which meets Australian Standards AS/NZS 4066 or AS/NZS 4499.
The following should also be considered to decrease the risk of eye injury in sport.
Functionally one-eyed players
Players who have poor vision in one or both eyes should wear appropriate eye protection. Consultation from an ophthalmologist or optometrist is essential.
Contact lenses
Contact lenses offer no protection. Therefore, players who wear contact lenses must also wear appropriate eye protection.
Obeying the rules
The importance of good sportsmanship and fair play should be emphasised. Coaches should develop clear rules for training and general conduct and always discourage violence or dangerous techniques.
Wearing protective equipment
Appropriate protective eyewear is a proven measure to prevent eye injuries in sports. Wearing appropriate protective eyewear is strongly recommended. Ordinary prescription glasses do not provide adequate protection.
The basic steps in choosing protective eyewear include:
- Using only eye protectors that are currently recognised under Australian Standard (i.e. AS/NZS 4066 – sports eyeguards or AS/NZS 4499 – sports helmet).
- Having an ophthalmologist or optometrist assist the athlete/player in selecting and fitting the appropriate protective eyewear.
Signs and Symptoms
- Tenderness
- Swelling
- Bleeding
- Bruising
- Double/blurred vision
There are different types of eye injuries that present with specific symptoms. These include:
Cuts or scrapes to the eyelids
Caused by fingernails and fingers and usually result in redness and pain, which should clear within a few days without serious long-term effects.
Blunt traumas
Caused by blows from fast moving projectiles (i.e. balls, racquets, sticks or fists/fingers). They can cause bleeding externally (i.e. black eye) or within the eye itself. Blunt traumas can also cause broken bones around the eye.
Penetrating injuries
In these types of injuries, a foreign body penetrates into the eyeball. This is most likely to occur when sports participants are wearing ordinary spectacle lenses as these can shatter on impact, possibly driving fragments into the eye.
Immediate Management
- Do not examine or touch the eye.
- Do not forcibly remove any foreign object from the eye. Gentle flushing with general saline to remove dirt/grit is reasonable. Do not administer any creams/drops before medical assessment.
- Pad the eye and gently tape or firmly bandage a sterile dressing to the injured eye. (N.B. if the player will allow, it is preferable to cover both eyes).
- Pressure to the injured site should be kept to a minimum.
- Keep the player comfortable.
- Consult a medical practitioner or eye specialist, or attend the emergency department at your nearest major hospital.
Rehabilitation and Return to Rlay
Athletes with a serious eye injury should be examined by an ophthalmologist and return to play only if the doctor says it is safe. The injured eye should feel comfortable and have adequate vision. The athlete should wear eye protection.
For a less serious injury, the team sports medicine professional can usually decide if the athlete can return to play based on the type of injury and how the athlete feels. Athletes should never use topical anaesthetics (pain medicines) so they can keep playing.
Acknowledgements
Sports Medicine Australia wishes to thank the sports medicine practitioners and SMA state branches who provided expert feedback in the development of this fact sheet.
Images are courtesy of www.istockphoto.com
Always Consult a Trained Professional
The information above is general in nature and is only intended to provide a summary of the subject matter covered. It is not a substitute for medical advice and you should always consult a trained professional practising in the area of sports medicine in relation to any injury. You use or rely on the information above at your own risk and no party involved in the production of this resource accepts any responsibility for the information contained within it or your use of that information.
